It's no secret that shifting hormone levels can affect everything from your mood to your menstrual cycle. And if you're a smoker or have high blood pressure, hormonal forms of birth control can increase your risk of stroke. Add it all together and for many women, the choice of contraceptive hinges on whether they want hormonal or nonhormonal birth control.
"We often use hormonal forms of birth control to manage premenstrual syndrome, cramps and heavy bleeding," says Katelyn Hartung, D.O., an obstetrician and gynecologist at Henry Ford Health. "The women who are seeking nonhormonal forms of birth control generally don't have a lot of complaints about their periods — and they don't want to disrupt their natural hormone levels."
Nonhormonal Birth Control: The Basics
Whether you're searching for nonhormonal methods of birth control for medical reasons, or because you don't want to muck with your body's natural hormones, there are many nonhormonal birth control options that can safely and effectively prevent pregnancy.
Of course, steering clear of sex altogether is the most effective form of birth control. But abstinence isn't the only nonhormonal option for birth control. Each method of contraception comes with advantages, disadvantages and varying degrees of effectiveness.
"Natural" forms of birth control
These so-called natural forms of birth control are the least reliable options. Still, many women find them preferable to other methods.
- Natural family planning: Also called fertility awareness, this method requires couples to avoid vaginal intercourse during the days surrounding ovulation. "If you have a predictable cycle, it's easy to pinpoint when you're ovulating," Dr. Hartung says. But for women who have unpredictable or long cycles, and those who are in perimenopause, natural family planning can easily result in a pregnancy. In fact, this method has a 24% unintended pregnancy rate. The reason: Sperm can live for up to five days inside the vagina and an egg survives for 24 hours after it leaves the ovary. So even with a predictable cycle, natural family planning can be a dicey proposition.
- Withdrawal: This approach requires the man to remove his penis from the woman's vagina prior to ejaculation. In theory, the approach is 96% effective. In real life that figure drops to 78% depending on the sperm’s ability to escape before ejaculation and, of course, timing. This method requires serious self-control on the man's part to pull out on time.
Chemical and barrier forms of birth control
Chemical and barrier forms of birth control prevent pregnancy by blocking sperm from reaching an egg.
- Spermicides: These are chemicals that kill sperm. Shortly before vaginal sex, spermicidal foams, creams or jellies are placed high in the vagina near the cervix using an applicator. Women can also place spermicidal films, suppositories, and tablets inside the vagina. The drawback: "The chemicals in spermicides can irritate the vagina," Dr. Hartung says. And since misplaced or ill-timed spermicide can derail its ability to block sperm, the actual effectiveness of spermicide hovers around 72%.
- Diaphragms: A diaphragm is a small, flexible cup that covers the cervix so sperm can't gain entry. Women have to be fitted for a diaphragm for it to be effective. Before inserting a diaphragm, you need to douse it with spermicide on both sides and around the rim. Then you compress the spring so it can be inserted into the vagina, and it pops open when it reaches the cervical area. The diaphragm is effective for up to 6 hours after insertion. With proper use, it's 94% effective.
- Cervical cap: This device works much the same way as a diaphragm, but it's smaller and only covers the cervix. It can be inserted up to 24 hours before intercourse and should remain in place for 8 hours after sex, but not more than 48 hours total. The effectiveness is only 86%, so it's not the best option if you're trying to prevent pregnancy.
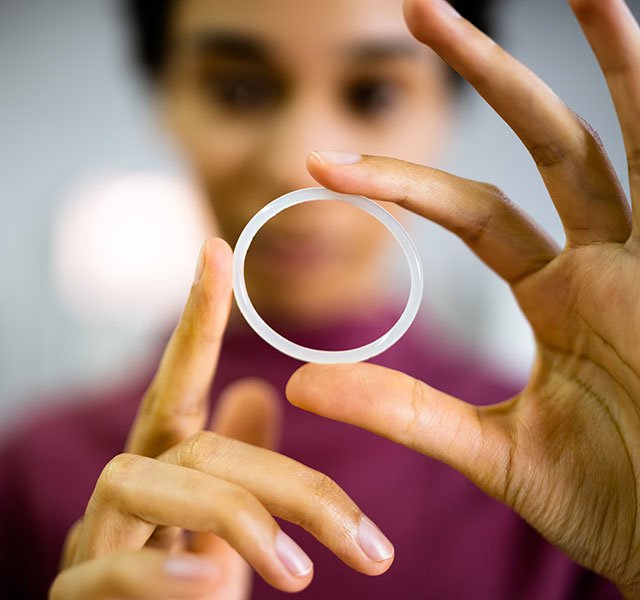
- Male and female condoms: Condoms are inexpensive and widely available. Male condoms have a theoretical effectiveness of 98% and an actual effectiveness of 85%. Female condoms, on the other hand, have a theoretical effectiveness of 95% and an actual effectiveness 79%. "The female condom is one-size-fits-all, which can make it awkward to use," Dr. Hartung says. Without a proper fit, the effectiveness drops off.
- Phexxi: A new option in nonhormonal birth control, Phexxi is a contraceptive gel that contains all natural ingredients (lactic acid, citric acid and potassium bicarbonate). It is not a spermicide. You just insert the gel into the vagina with an applicator (like a tampon) and it keeps the vagina acidic, which immobilizes sperm and prevents them from swimming up the vaginal canal. The effectiveness rate is about 86% for typical use and some women experience vaginal irritation after use.
Long-term and permanent forms of nonhormonal birth control
If you're looking to protect against pregnancy for years or longer, you have a couple of options:
- Copper intrauterine device (IUD): An IUD is a small, T-shaped device that sits inside the uterus to prevent pregnancy. Getting an IUD is an in-office procedure where your doctor inserts the device into your uterus. Once in place, an IUD provides reliable birth control for 10 years. And it's remarkably effective, with a failure rate of only 0.8%. The copper IUD is also the only nonhormonal form of emergency contraception. If a doctor inserts the device within five days of unprotected sex, you'll reduce your odds of getting pregnant by 99.9%. IUDs are among the safest, most effective, and least expensive reversible contraceptives available. The only drawback: "For some women, the copper IUD can make periods heavier and cramps more intense," Dr. Hartung says.
- Sterilization: Sterilization is a permanent form of birth control. Surgical forms of sterilization include tubal ligation (where a doctor ties off a woman's fallopian tubes, which prevents an egg from reaching the uterus) and vasectomy (where a doctor cuts and closes off a man's vas deferens, which prevents sperm from coming out). Both procedures are highly effective, but tubal ligation is more costly and complicated, unless you get your tubes tied during a cesarean section delivery.
Weighing Your Contraceptive Options
When it comes to hormone-free birth control, the best option is the one that feels comfortable to you — and that you’ll use with confidence every time you have sex. The key considerations when you make contraceptive decisions:
- Your health
- Whether you want kids in the near future, or ever
- If you need to protect against sexually transmitted infections (STIs)
- How often you have sex
"I like to provide patients with all of the options up front, so we can discuss which ones are best for their unique circumstances," Dr. Hartung says. "The idea is to find the option that is safe, effective and won't cause bothersome side effects."
Remember, too, that with the exception of permanent forms of birth control, like sterilization, women can switch methods as needed. You have options. So never hesitate to ask your doctor to help you understand the pros and cons of every available method.
Subscribe today to receive weekly emails of our latest tips.
To find an OB/GYN at Henry Ford, visit henryford.com or call 1-800-436-7936.
Dr. Katelyn Hartung is a OB/GYN who sees patients at Henry Ford Medical Center - Royal Oak.